|
Author(s): John K. Chae BA (1), Wende N. Gibbs MD (2)
Affiliation(s) (1) Department of Neurological Surgery, New York Presbyterian Hospital-Weill Cornell, New York, NY, USA (2) Department of Radiology, Mayo Clinic, Scottsdale, AZ, USA Date Submitted: 1 June 2021 Date Published: 7 January 2022 Abstract Over the past few decades, there has been a rapid advancement in neuroimaging capabilities, and we now have a wide range of tools available for both clinical and research applications. The goal of this article is to review fundamental concepts of neuroradiology with a focus on computer tomography (CT) and magnetic resonance imaging (MRI) for medical students interested in the clinical neurosciences. Computed Tomography (CT) Background Common to most Emergency Departments and inpatient centers, CT of the head or spine is often the first imaging modality used because of its low cost, high information yield, and relative speed. CT scans can be thought of as “3D” x-rays – instead of using a fixed source of x-ray beam, a CT scanner uses a rotating source of multiple x-ray beams that ultimately result in multiple 2D image slices of a target region. CT scans can be performed with or without intravenous (IV) contrast. Non-contrast CT, easy to obtain and thus more common, is generally first-line in emergency situations, especially if there is any concern for acute bleeding or a progressive space occupying lesion in the thecal sac or intracranial space. CT with IV contrast is typically for patients with contraindications to MRI who need radiographic evaluations of neoplasms or vascular malformations. CT Head Indications There are several situations in which CT scans of the head are particularly useful:
*When evaluating CT of the head, it is important to differentiate fractures from the normal cranial sutures (lambdoid, coronal, etc.) of the skull. This can be done by comparing potential fracture site to contralateral side for asymmetry. Occasionally, a CT scan is obtained to rule out increased intracranial pressure (ICP) in patients with suspected meningitis prior to performing a lumbar puncture. Performing a lumbar puncture on a patient with an increased ICP may lead to cerebral herniation and death. However, some studies have shown that obtaining a CT head first may delay diagnosis and initiation of appropriate therapy (Hasbun et al. 2001). Thus, for suspected meningitis cases, a CT head should be obtained if there are additional concerning signs of elevated ICP or other risk factors, such as altered mental status, focal neurologic deficits, papilledema, immunocompromised state, recent seizure, and/or history of other CNS disease. Contraindications There are relatively few contraindications for CT scans. Since it involves X-ray radiation, it is generally not used for young children and pregnant patients. When using CT with contrast, allergies to iodinated contrast material and underlying renal disease are potential contraindications. In non-emergent situations where these contraindications may be suspected, it is important to obtain renal chemistries (i.e., basic metabolic panel) to evaluate for elevated creatinine, as well as query the patient’s allergy and social histories. Signal Density The actual images produced by CT scans are radiodensities interpreted by a computer, which reflect how much of the original x-ray beam is attenuated (i.e. weakened) as it travels through a given medium. This is reflected by an arbitrary determination of density as measured by Hounsfield Units (HU) (i.e., more density equals higher HU). Hyperdense (high attenuation) areas are brighter relative to their surrounding brain, and they usually correspond to acute blood, bones, and areas of calcification. It is important to note, however, that while acute blood is hyperdense on CT scans, subacute blood often appears isodense to the surrounding brain (i.e., similar in grayscale appearance to the brain parenchyma). Hypodense (low attenuation) areas are, on the other hand, dark compared to adjacent brain, and they are usually due to edema, air, or subacute/chronic stroke. There are two types of brain edema: vasogenic and cytotoxic. Vasogenic edema is extracellular fluid accumulation due to disruption of the blood-brain barrier (BBB) from various causes, including neoplasm, abscess, and inflammation. This type of edema mainly affects the white matter. Cytotoxic edema is due to intracellular fluid accumulation associated with cellular injury and death. Here, the BBB is intact, and it affects both the white and gray matter. This type of cellular injury is generally caused by cerebral ischemia. An example of how blood typically appears on a CT Head without contrast in subdural hematoma is shown below: Acute Phase (0 to 2 days from injury): Appears hyperdense, i.e., “bright”. Subacute Phase (>2 days to <2 weeks from injury): Can appear mixed, typically isodense and can be missed. Chronic Phase (>2 weeks from injury): Appears hypodense, i.e., dark as blood changes to a clearer liquid, which appears like a hygroma. CT Head Interpretation When reading a CT head, there are three important considerations to keep in mind.
In an acute head trauma situation, it can be useful to assess emergent CT of the head using a B-C-B-V-B technique:
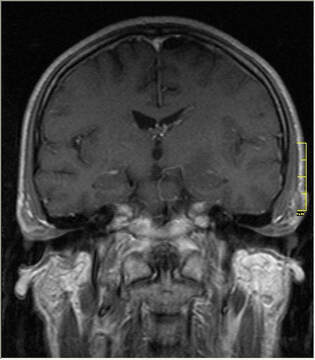
CT Spine Interpretation A helpful mnemonic for systematically interpreting a CT spine is ABCS: A: Alignment. On the mid-sagittal cut, there should be 4 smooth curves without any angulation – (1) anterior vertebral line (anterior surface of the vertebral bodies), (2) posterior vertebral line (posterior surface of the vertebral bodies and anterior surface of the spinal canal), (3) spino-laminar line (posterior surface of the spinal canal), and (4) posterior spinous line (posterior tips of the spinous processes). B: Bones. Look for any fractures, changes in bone density, lytic lesions, and degenerative changes. C: Cartilage. Examine the intervertebral spaces for possible asymmetry, widening, or narrowing. S: Soft tissue and spinal canal. Soft tissues surrounding the vertebra and the spinal canal should be symmetrical. It is important to note that the vertebral column has a complex associated ligamentous network, which is difficult to observe on a CT scan. Magnetic Resonance Imaging (MRI) Background MRI provides much more detailed images of the brain parenchyma and other soft tissues. MRI scanners produce a magnetic field that aligns protons in the body and subsequently apply a radiofrequency pulse, which excites protons in the target image area. When MRI machines stop applying this radiofrequency pulse, the excited protons return to their alignment with the magnetic field and release previously absorbed energy, which is converted to images. Given this different imaging method, we use the terms hyperintense and hypointense to refer to bright and dark areas of the image, respectively (note that we use “density” for CT and “intensity” for MRI, think “I” in MRI stands for “intensity”). Because the human body contains many water molecules (and thus protons), MRI is able to capture very detailed images without the use of ionizing radiation. Additionally, various MRI sequences (i.e. different methods of data acquisition and image rendering) may be used to better characterize and evaluate different tissue types. The downsides to MRI are cost, imaging time, and number of contraindications relative to CT scans. Indications for MRI For most brain pathologies, MRI has a greater sensitivity and specificity than that of CT. Thus, MRI is used to better identify and localize brain tumors (particularly those that enhance with gadolinium contrast, i.e., the “ring-enhancing lesions”*), infection, stroke (particularly older lesions), and hemorrhage. It may also be used to diagnose seizure disorders, neurodegenerative diseases, inflammatory diseases (such as multiple sclerosis), and congenital disorders. Spinal indications are similar, however MRI is commonly obtained if there is a concern for ligamentous injury and instability in acute trauma or for acute epidural hematoma in the setting of signs of cauda equina (i.e., saddle anesthesia, urinary incontinence, lower leg neurological deficits). Contraindications Presence of certain implants, such as cochlear implants and vascular stents, can be an absolute contraindication due to the strong magnetic field of the MRI machine. However, MRI-compatible metal implants are becoming increasingly available, and device documentation should be cross-referenced prior to imaging. Since most MRI machines require the patient to remain still in a tight space, claustrophobia is a common relative contraindication to obtaining MRI; however, sedation may be used when MRI is essential (i.e., a single dose of benzodiazepine). Similarly, obtaining MRI for young pediatric patients often requires sedation. Use of newer open MRI machines may help reduce claustrophobia, but due to the use of weaker magnets, image acquisition is slower and image resolution is lower. Lastly, MRI for critically ill and emergency patients is often difficult due to limited capacity for monitoring and patient access inside MRI machines during the time-consuming image acquisition process (CT of the head takes ~15 minutes while an MRI of the brain can take up to an hour or more). Gadolinium Contrast MRI can be performed with or without IV contrast – of which, gadolinium-based contrast agent (GBCA) is most frequently used. Typically, GBCA is unable to permeate the BBB, and thus contrast enhancement in the brain parenchyma signifies disruption of the BBB. The major etiologies of BBB disruption and GBCA enhancement can be remembered by the mnemonic, MAGIC DR Lick (metastasis, abscess, glioblastoma, infection, inflammation, or infarct (subacute), contusion, demyelinating disease, radiation necrosis, and lymphoma). Suspicion for these conditions should prompt consideration for ordering MRI brain with contrast. Interpretation: Common MRI Sequences and Types There are multiple sequences to an MRI, interpreted as different-appearing images by the computer depending on the anatomy and pathology. In the T1 sequence, fluid appears hypointense (i.e. dark) while fat appears hyperintense (i.e. bright). Thus, CSF is hypointense and lipid-containing tissues, like myelinated white matter and subacute blood products, are hyperintense. The T1 sequence is great for assessing normal anatomy because white matter appears white and gray matter appears gray. Often, brain lesions have a higher water content than that of normal brain and appear hypointense. When this occurs, T1-weighted images do not contrast well between normal and abnormal tissues. In this case, a T2 sequence is usually more helpful. In T2-weighted images, both fluid and fat are hyperintense. CSF is white, white matter is dark gray, and gray matter is light gray in these images. Most brain lesions with increased water content will appear bright on T2, providing good contrast between normal and abnormal tissues. T2 sequences are also highly anatomic, meaning they allow for an initial evaluation of asymmetry. Often, attending neurosurgeons will want to have the T2-sequence pulled up first alongside a T1 post-contrast if available. Fluid attenuation inversion recovery (FLAIR) is a special type of T2 sequence in which specific CSF signals are suppressed and thus appear dark while other non-CSF fluid signals (e.g. edema) are still bright. This is helpful when T2-weighted images poorly distinguish between abnormal hyperintense signals and the hyperintensity of CSF. FLAIR is great for highlighting pathologic areas of the brain, particularly those with perilesional edema. Diffusion-weighted imaging (DWI) is a particularly useful type of MRI for evaluating acute ischemic stroke. It works by measuring the random (Brownian) motion of water molecules and calculating the apparent diffusion coefficient (ADC), which reflects the degree of water diffusion at a particular location. On DWI, the amount of water diffusion (ADC) is inversely proportional to signal intensity. Thus, conditions that cause cytotoxic (intracellular) edema, such as acute infarction, abscess, and lymphoma, restrict diffusion and appear hyperintense. Functional MRI (fMRI) assesses cortical activity by measuring changes in cerebral blood flow to a particular area. Generally, more active areas of the brain receive increased blood flow, which is reflected on fMRI. Clinical use of fMRI is quite limited, but it may be useful in preoperative mapping of functional areas of the brain that must be avoided intraoperatively. The majority of fMRI use is in research, as it is a valuable tool in mapping activity and localizing function. Cerebrovascular Imaging Cerebrovascular imaging can be obtained using CT angiography (CTA), MR angiography (MRA), transcranial Doppler (TCD), or endovascular cerebral angiography. CTA is the administration of IV contrast combined with CT technology. Like normal CT scans, CTA exposes the patient to ionizing radiation, but it can be done relatively quickly and is highly useful for diagnosing subarachnoid hemorrhage from a suspected aneurysm or vascular malformation. MRA, on the other hand, can be performed with or without contrast, but it is not as time efficient and has MRI-specific contraindications. TCD is a cost-efficient, quick, noninvasive bedside ultrasound technique but has several limitations. It is highly operator-dependent and often requires adequately trained sonographers. Illustration of the cerebrovascular anatomy is limited, and it is performed through a bone window that varies greatly in adequacy among patients due to anatomic variations. TCD is commonly used in the neurological intensive care unit to assess the risk of vasospasm after aneurysmal subarachnoid hemorrhage. Endovascular cerebral angiography is considered the gold standard of cerebrovascular imaging. In this more invasive approach, a catheter is inserted into a peripheral artery – usually the femoral or radial artery – and advanced under fluoroscopic (X-ray) guidance to the region of interest where contrast material is injected. Then a series of X-ray images are taken to illustrate the anatomy of the blood vessels in real time while the contrast dye is moving through the vessels. Complications include contrast allergies, hematoma formation, infection, aneurysm or pseudoaneurysm formation, and atherosclerotic embolization. A Few Notes About How to Excel on Sub-Internships and Rotations Understanding the fundamentals of neuroradiology are important not just for neurosurgery residents and students to master for clinical excellence, but also allows an opportunity to set oneself apart during a sub-internship or rotation. While this list is not exhaustive and is highly site-dependent, a couple neuroimaging-specific pieces of advice are as follows:
Conclusion With advancement and wider availability of neuroimaging, the role it plays in patient care and neurosurgical practice is becoming increasingly imperative. CT and MRI are commonly used neuroimaging modalities, and they have many different useful applications. Thus, it is crucial to understand their underlying fundamental concepts, indications, contraindications, and principles of interpretation. Medical students should become familiar with their basics to set themselves apart on rotations as well as lay a foundation for residency training. References 1. Ahmad Z, Mobasheri R, Das T, et al. How to interpret computed tomography of the lumbar spine. Ann R Coll Surg Engl. 2014; 96(7): 502-507. 2. Greenberg MS. Handbook of Neurosurgery, 9th ed. New York: Thieme, 2020. 3. Griffith B, Kelley BP, Patel SC, Marin H. Cerebrovascular Imaging (CT, MRI, CTA, MRA). In: Hans SS, ed. Extracranial Carotid and Vertebral Artery Disease: Contemporary Management. Cham: Springer International Publishing; 2018:85-111. 4. Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed Tomography of the Head before Lumbar Puncture in Adults with Suspected Meningitis. N Engl J Med. 2001; 345:1727-1733. 5. Hendricks BK, Eitel JA. Introduction and Review of Imaging Modalities. The Neurosurgical Atlas. Accessed August 30, 2020. DOI: https://doi.org/10.18791/nsatlas.v1.02 6. Lin A, Rawal S, Agid R, Mandell DM. Cerebrovascular Imaging: Which Test is Best? Neurosurgery. 2018; 83(1): 5-18. 7. Michinaga S, Koyama Y. Pathogenesis of Brain Edema and Investigation into Anti-Edema Drugs. Int J Mol Sci. 2015; 16(5): 9949-9975. Image License: Publicly available from Wikimedia Commons used with permission through CCA-share alike 3.0, credit: Nevit Dilmen. Conflicts of Interest: The authors report no conflicts of interest concerning the material or methods used to develop this manuscript. Acknowledgements: No acknowledgements Editor(s) Abdullah Uddin, BS Senior Student Editor Section Editor for Spine and Neurotechnology Michael W. Kortz, MBA Interim Editor-In-Chief Brain & Spine Report Medical Student Neurosurgery Training Center Comments are closed.
|
Categories
All
Archives
October 2023
|


1/5/2022